By Dr. Mansoor Khan
The business of health care is changing; faster than most of us would like. The Urgent Care sector is projected to grow to over $26 Billion per year by 2023. Between 2007 and 2016 the number of claim lines for Urgent Care grew by 1,725%. Interestingly from 2012 to 2017 the number of patients using non-face-to-face services grew by 600% and is expected to accelerate. You see the pattern(s)?
There are actually 2 primary takeaways from this data:
1) Urgent care is taking business from traditional brick-and-mortar care (remember this term from the dot com days?), yes, it is finally happening to medicine!
2) The non-face-to-face visit is growing even faster. I very purposefully use the term non-face-to-face rather than e-visit or telemedicine because the later 2 terms have a lot of reimbursement limitations that make them of very marginal value for the average practice. However, the non-face-to-face visit encompasses a number of CPT codes that can generate over $50,000 per month of additional revenue for each physician.
There is a lot of complexity here and we will dive deeper into that in subsequent posts, but suffice to say that to thrive in this new world you need to be thinking like a consumer business that has to meet its customers where they are and not where you might want them to be. – BUT do so in a way that increases your revenue and decreases the amount of work you are doing.
Stay tuned…
Persivia Webinar April 5, 2016, 3:00 pm CST
Dr Mansoor Khan will give a webinar on Chronic Care Management, sharing his thoughts on success and challenges in implementing these services. Further details are coming.
What Comes Next for Chronic Care Management?
By Mansoor Khan, CEO, Persivia
The Chronic Care Management CPT code (99490) allows providers to collect approximately $42 per qualified patient per month for providing 20 minutes of non-face-to-face care management services to Medicare beneficiaries that have at least 2 chronic conditions. This, as with most new CMS initiatives, has as its ultimate goal the objective of improving patient outcomes and satisfaction. How do we get from this fee- for-service reimbursement to improved outcomes?
The Grand Plan
CMS has an overall plan that moves the healthcare system into value-based payments at a breakneck speed. In order to get there, CMS has defined 4 categories of payments which are as follows:
• Category 1—fee-for-service with no link of payment to quality
• Category 2—fee-for-service with a link of payment to quality
• Category 3—alternative payment models built on fee-for-service architecture
• Category 4—population-based payment
As shown in the figure below, CMS plans to have 90% of all payments at a minimum linked to quality of care (as measured by CQM scores) by 2018 and by then at least 50% of payments will be under alternative payment models which typically will link them to patient outcomes. That is about $500 billion!
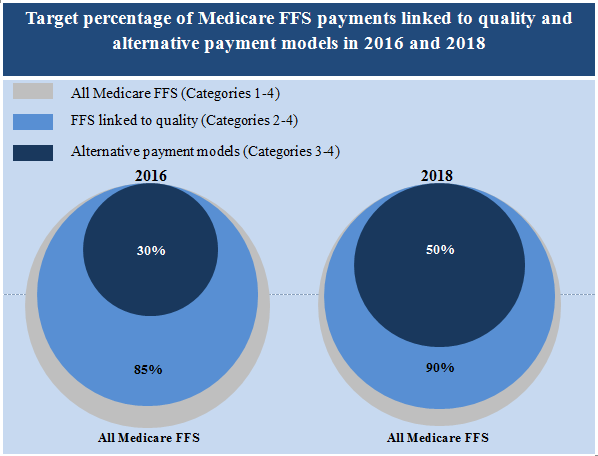
What does this change mean for the new fee-for-service CCM code? Basically, it means that this code will not stay the same for very long. We expect that soon various Clinical Quality Measures (CQMs) will start to be applied to the patients receiving this service and within a year or two after that this population will need to start demonstrating improved clinical indicators. Of course politics could shift this change, but the overall trend will remain the same.
What Does this Mean for Physicians and Hospitals Now?
Knowing where the train is headed, we must get aboard with the right equipment, otherwise we won’t make it to our destination. CMS has created a nice FFS ramp to ease providers into this new world. However, the decisions providers make on the tools to use for the FFS part will have a great deal of impact on their success as these codes transition towards outcomes. The vendor/partner that the provider picks now will impact numerous factors down the line, including:
• Impact on quality scores
• Impact on care standardization (acute and post-acute)
• Impact on driving additional visits, labs etc.
Keep in mind that one of the largest factors impacting the quality of care is the variation in the standard of care. This is especially true for the post-acute environment where the quality of care is greatly influenced by the training and dedication of the clinical and support personnel involved. Significantly, and as the manufacturing world learned in the ‘80s and ‘90s, until you reduce the variability in the processes being applied, you cannot improve overall performance. To put it another way, if your shots are all over the target, trying to improve accuracy is difficult. Once you have bunched your shots so they all fall in one area then getting them to hit the center of the target is a relatively simple matter. Similarly, once we have reduced the variability of care by controlling and influencing care delivery by providing – based knowledge at the point of care, we can start making significant strides towards improved clinical indicators and outcomes. But, how can we do that?
What Tools Should be Selected?
When providers sit down to select a CCM partner they need to think about how their partner’s Care Management (CM) platform will impact the factors mentioned above. There is one set of capabilities that rise above all others in importance when one wants to achieve the goals mentioned above. This is the depth and breadth of the clinical knowledge (or decision support) embedded within the CM system workflows. Crucially, the CM system needs to be able to achieve this in real-time and do so within the clinical workflows. Unless the CM system has the ability to access a very large body of evidence-based knowledge, and can inject that into the workflow as a set of Alerts, Goals and Assessments in real-time, one will not achieve one’s goal of reduced variability and improved care.
So, as you move into providing CCM services and select a partner to help you in this journey, make sure that they also value improving the quality of care as much as you do.
Laying the Groundwork for Implementing a Chronic Care Management Program
By Mansoor Khan, CEO, Persivia
First the numbers:
- 45% of the world’s population is affected by chronic disease
- 60% of worldwide deaths are caused by chronic disease
- 4% of the global annual GDP represents the economic burden associated with chronic disease
- 17% of the US GDP is spent on healthcare, and chronic disease makes up 75% of this expense
- 80% of chronic disease can be prevented
The numbers are staggering, so what do we do about this? Well, as individuals we can exercise more, eat better and lose weight, but that is not what I am asking. I mean what do we do as a society? Fortunately, the healthcare industry as a whole is working on the problem. However, in this, and successive blogs, I will focus on the path that CMS is taking to address the issue of Chronic Disease Management.
What is CMS Doing About it?
As we all know now, CMS launched the now CPT code (99490) which pays providers an average of $42 for 20 minutes of non-face-to-face contact with Medicare Beneficiaries diagnosed with 2 or more chronic conditions. We are now over 10 months into the program. So how is it going? Or to (mis)quote Field of Dreams, “If you build it will they come?”
According to a recent survey by PYA, as of October 2015 only about a quarter of eligible providers had launched CCM programs and only about half of those had actually billed for those services. According to CMS, approximately 100,000 patients (out of a possible 25 million) had been billed for so far. Given that providers are finally being reimbursed for work that they are already doing, why is adoption so low?
There are a number of reasons for this low response. They generally fall in the following three categories:
- Providers aren’t comfortable that they understand the rules and don’t have the time to do the necessary research
- Providers don’t have the resources needed to perform the service
- Providers do not believe that they can make money performing this service
These are of course valid concerns and even more so for small practices.
I won’t spend much time explaining what the rules and regulations are but you can find a very good summary on the CMS website. What I do want to point out is that the free market and good old entrepreneurship has come to the rescue. There are now many companies that will provide a combination of software and services to help the provider deliver this service. However, not all such companies are created equal. Many are fly by night operations that are trying to do a dot com like land grab by launching a purely manual, bare bones service and signing up as many providers as fast as they can and then worrying about the quality of the service at a later time. Many are basically call centers that do not have the CMS required technology and are just peddling bodies on the phone, and still others that just provide software for use with the service. Depending on your specific circumstances, any of these may be the right partner for you. Additionally every EHR supposedly has a Care Management module in their system. So…
7 Questions to Ask a CCM Vendor
If you are among the 74% of providers who haven’t taken action on deploying a CCM program, what should you do? If you are hesitating because of any of the three reasons above, then the solution might just be to select a care management service provider that offers a turnkey service. In any case, you will need a Care Management (CM) software system. However, as in everything else in life, all are not created equal.
Below are 7 questions you should a potential vendor during your care management software selection process:
- Do they have a software system for care managers to use that can track and maintain a longitudinal health record for each patient (a Medicare requirement)?
- Does their CM system accept patient summaries in the form of a CCD or CCDA (a Medicare requirement)?
- Does their CM system track care provider time and maintain a log of all activities in case there is a CMS audit (remember you are the one billing CMS and will be held responsible for any inaccuracies or shortcomings)?
- Does their CM system provide decision support tools that help the care managers track where the gaps in the care of the patient are, what assessments need to be performed, and what goals need to be set for each patient. This is critical to ensure that what CMS is trying to do (I.e. Improve the care of the sicker patients) actually gets done?
- Are they able to connect to your EHR system and identify the patients that qualify for the CCM program?
- Do they provide 24×7 coverage?
- Are their Care Managers trained in providing evidence-based, patient-specific care management?
Stay tuned for our Blog post on what comes next?
Population Health, Care Management & Clinical Surveillance at the Heart of HIMSS 2015 Buzz

CEO Dr. Mansoor Khan Provides His Observations from the Show Floor
Q: What did you take away as the biggest changes ahead for the healthcare industry in 2015?
A: Population health management and how providers and clinicians can more effectively manage patients, and their data, were some of the main issues that I had addressed at the show. In the past, we had focused on the provider data, which essentially was “dirty data” that needed better ways to be captured, normalized and then interoperate across healthcare systems and into clinical workflows. But on the horizon, the biggest challenge will be around consumer data, where cognitive computing and machine learning will play a big role in aggregating and incorporating these new, and vast, consumer-driven data.
Also a big healthcare change that was discussed was managing patients with two or more chronic conditions. Under a new rule published by CMS, which went into effect on January 1, 2015, clinicians who dedicate at least 20 minutes to care management services during a 30-day period will be paid $41.92 a month, including non-face-to-face care. This new regulation was a huge topic during the show. Especially with new health care models shifting from inpatient to more outpatient services, home-based chronic care management is a natural evolution for the healthcare industry. By allowing for non-face-to-face care, this will keep patients in their homes and with their caregivers, and will be a tremendous leap forward in the way that patients and their clinicians communicate and collaborate on chronic care treatment.
Q: What are the major hurdles that were discussed on advising providers concerned about satisfying the new CMS regulations for chronic care management?
A: We talked to a lot of ACOs and hospital systems about the challenges that will come with tracking billable time, handling the billing process and reimbursements, to even locating, and providing clinician resources for the required monthly care management and patient interaction. Technology will continue to be the linchpin to the success of these chronic care programs. Having the right population health platform is also key. It has to be comprehensive, accessible and meaningful. Providers need to easily identify eligible beneficiaries for enrollment, have access to disease registries for advanced tracking and deploy real-time evidence-based alerts to close crucial care gaps. Few products on the market today are able to capitalize on this opportunity, and those that can, will have a great competitive advantage.
Q: What were some additional trends emerging from the show?
A: It seems that the biggest change from the providers point of view is this dramatic shift from in-patient services to ambulatory services. Hospitals that do not have a solid plan on how to shift their models accordingly will face big challenges. CMS is already promulgating new regulations that will both force and enable these changes. Additional CMS regulations are coming to infection control and managing antimicrobial stewardship. I talked to many hospitals that are considering implementing a real-time clinical surveillance solution to help prevent and contain hospital-acquired infections (HAIs) to avoid escalating CMS penalties. This is a huge concern, and these penalties have just increased from 2% to 3% this past year. In 2015, CMS had also expanded the scope of reporting HAIs from not just the ICU but hospital-wide. It will become ever more critical to implement automated real-time monitoring tools that will mitigate these risks by quickly identifying HAIs, which in turn, will significantly cut down on the instances of re-admissions.
Q: Any final thoughts from HIMSS 2015?
A: The health care industry continues to evolve around patient-centric solutions as we transition from fee-for-service to value-based care. Meaningful Use regulations have made great strides, and will continue to become even more important with the coming of Meaningful Use Stage 3. Making all health records digital is positive progress, but interoperability and managing this vast amount of patient data remains problematic. This is where Big Data and cognitive computing will play an active role in shaping this next stage of Meaningful Use. On the whole, and despite some familiar HealthIT challenges, there have been great gains made in the last few years, and patient outcomes should remain a top priority for providers. By focusing on improving the patient experience and better chronic care management, I think 2015 will be a truly transformative year in healthcare.
By Fauzia Khan, MD, FCAP
As the healthcare industry continues a positive shift toward value-based care and away from the fee-for-service model, payers and providers are starting to look at patient engagement and managing chronic conditions very differently. Previously, disease management was measured more by associated cost such as procedures ordered, in-patient stays and re-admissions, and patient engagement typically consisted of generalized letters that described their disease and standard therapies. These letters were a one-way communication and hardly fulfilled the notion of “engagement.”
There have been great strides made recently in developing patient-centric, IT solutions such as electronic health records, personal health records, health information exchanges and clinical decision support platforms. These platforms are finally enabling physicians, providers and payers to improve their care coordination and communications, while increasing the quality of care for patients. While this is definitely a welcome advancement for healthcare IT, a very important group is conspicuously left out of the conversation — actual patients. But that too is starting to change.
With ubiquitous use of mobile devices and more people opting for home healthcare, many patients want to take a more active role in managing their own health, so why not invite them into the conversation? As technology companies work to develop cutting-edge, patient-centric solutions, it will become increasingly more important to actually involve the patient in the process of developing their individualized treatment plan. Empowering patients in managing their own care becomes even more important with the prevalence of chronic conditions.
Recent data shows that more than 145 million people, or almost half of all Americans, live with a chronic condition. That number is projected to increase by more than one percent per year by 2030, resulting in an estimated chronically ill population of 171 million. Today, chronic diseases such as diabetes, cardiovascular disease, COPD, and hypertension are among the most prevalent, costly, and preventable of all health problems. Seven out of every 10 Americans who die each year (more than 1.7 million people) have one or more chronic diseases and 80% of chronic diseases are preventable with appropriately tailored treatment and wellness plans.
As of January 1, 2015, the Centers for Medicare & Medicaid Services (CMS) started paying physicians for delivering care management to their Medicare patients with two or more chronic conditions. The newly created CPT code, (99490) reimburses providers for spending at least 20 minutes per month on care, including non-face-to-face interactions, with their patients. Eligible providers and qualifying clinicians will be reimbursed at approximately $42 per patient, per month.
With new regulations pushing the healthcare industry forward to ensure better patient engagement and care, it’s clear that changing the way care is currently delivered in the hospital and beyond is starting to become a necessity. The vision is clear: identify efficiencies, while maintaining high clinical quality to ensure delivery of the right care, at the right place and time. However, the execution seems to be elusive, and most providers and payers do not know where to even start.
This requires collecting, analyzing and sharing information, working across silos and engaging patients in an unprecedented and innovative manner. Data needs to be recorded from all sources, from the EHR to the Apple watch. And this data needs to be bi-directional, enabling real engagement between patients and clinicians. In turn, it is our responsibility as technology providers to develop solutions that work together to enable transparency, collaboration and information-sharing. Like many shifts in healthcare, changes won’t occur overnight. It will take time. However, by making efforts today to move treatment closer to the individual, and involving patients in the development of technologies enabling this shift, we as an industry can accelerate decisions that can lead to better outcomes.
About Dr. Fauzia Khan
Fauzia Khan, MD, FCAP is chief medical officer and co-founder of Alere Analytics. Dr. Khan provides direction and leadership to develop practical and scalable technologies that allow clinical decision support and analytic capabilities to be seamlessly incorporated into clinical workflows. She has expertise and passion for algorithm design, knowledge acquisition and engineering as well as data mining and leveraging these capabilities to improve outcomes. Prior to forming DiagnosisOne, Dr. Khan was the director of informatics at UMass Memorial Medical Center with ten years of experience in the hospital practicing pathology. She is the author, editor and primary visionary of the “Guide to Diagnostic Medicine” (Lippincott Williams & Wilkins, 2002).
Improving Care Collaboration and Making Data Available and Actionable across the Connected Healthcare System
The mandate to embrace technology has been driven by federal government regulations, as well as disruption of the traditional fee-for-service model. Although we have started to embrace this model in the clinical world, what if these technology platforms could also be effectively used across the entire continuum of care, from the hospital to the home?
Over the past decade, technology innovations have continually pushed the boundaries in the healthcare industry. According to a CDC report (figure 1) in February 2015, it shows a dramatic increase in EHR adoption. This is due, in part, to the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, which provided incentive payments to eligible hospitals and providers that demonstrate the meaningful use of a certified electronic health record (EHR) system, but it also shows the pent up demand and the inevitable paradigm shift that is coming to the healthcare industry that patient data needs to be accessible, available and actionable.
Figure 1. Hospital emergency departments with an EHR system: United States, 2006–2011
NOTES: All trends were significant (p < 0.05). EHR is electronic health record. “Any EHR system” is a medical or health record system that is either all or partially electronic. Emergency department estimates are based on a question indicating the department “uses” an EHR. Estimates for a basic system prior to 2007 were not included, as not all data elements were collected. A basic system had all of the following functionalities: patient history and demographics, patient problem lists, physician clinical notes, comprehensive list of patients’ medications and allergies, computerized orders for prescriptions, and ability to view laboratory and imaging results electronically. SOURCE: CDC/NCHS, National Hospital Ambulatory Medical Care Survey, 2006–2011. Adoption of a basic EHR system by hospital EDs increased from 19% in 2007 to 54% in 2011.
Significant challenges remain with aggregation, data capture and normalization capabilities in the hospital and ambulatory settings, however we are beginning to see some improvements, this finally allows for better care coordination across the continuum of care. The addition of clinical decision support (CDS) and real-time analytics becomes even more critical, thus enabling clinicians to develop the best treatment plans for each patient, using intelligent and actionable information. Another driving force to deliver better care coordination and communication is actually coming from the consumer market. Recent technologies such as wearables have allowed patients to take a more active role in their own care, empowering them to make better, healthier decisions. The FDA estimates that 500 million people worldwide will use a health app by 2015, and estimates predict that by 2017, the global mobile health and wellness app market will be worth $26 billion. Most of the revenue, about 84 percent, will come from related services and products like wearables, such as Fitbit and Jawbone, and also future technologies like the new Apple Watch.
Data at the point-of-care, whether in the home, in-patient or ambulatory setting should be actionable, comprehensive, and increasingly accessible to all key stakeholders including patients, physicians, and payers. Whether that data is delivered through an HIE, EHR, or a smart device. In time, once we move treatment closer to the individual, this will close crucial care gaps, provide greater visibility, and accelerate decisions that lead to better outcomes.
If the last decade was focused on inpatient, outpatient, and ambulatory data integration and interoperability, the next several years should focus on creating the Connected Healthcare System, which includes the home. With mobile technologies, ubiquitous Internet, and smart devices, the boundaries between home, hospital, and ambulatory and long-term care facilities will blur.
With patient-specific and real-time information accessible at the point-of-care (the definition of which will also change), physicians could better manage common chronic conditions and patient populations. In addition to clinical decision support (CDS), another necessary layer to develop would be around analytics. CDS would empower clinicians to make more informed, evidence-based decisions, while real-time analytics would allow clinicians to view and analyze at-risk populations from both a preventative and interventional perspective. Analyzing patient populations and outcomes provides vital information for physicians that can significantly impact patients by triggering earlier interventions, reducing avoidable errors, and improving overall health outcomes.
A fully realized Connected Healthcare System is still in development, but it is certainly within our reach. As we move toward more integrated technologies across hospitals and lab systems, we need to also spend our resources on developing a home network that can provide evidence-based data and real-time alerts to providers, patients, physicians, and even network managers. Once this integration takes place, the healthcare industry can focus its attention where it belongs—on better managing patients and populations.
Fauzia Khan, MD, FCAP is chief medical officer and co-founder of Alere Analytics.